E/M Calculations
If you haven't already done so, please read Electronic Medical Record (EMR) Overview and Using Charting Templates before proceeding.
The EMR Glossary explains a number of EMR specific terms.
Summary
The Charting templates and wizards have been designed to assist clients in arriving at the most accurate Evaluation and Management (E/M) Services coding, for purposes of insurance reimbursement. The coding rules were defined in general terms by CMS, and there have been numerous publications written to lay out the specific guidelines for coding. Net Health has relied heavily on the AMA publication, Current Procedural Terminology, Professional Edition, which is updated each year. In addition, we have incorporated information from the 1995 Documentation Guidelines for Evaluation and Management Services the 1997 Documentation Guidelines for Evaluation and Management Services, and the 2021 Documentation Guidelines for Evaluation and Management Services (each of which is available to clients from Net Health), as well as various coding audit worksheets and pocket reference guides contributed to us by our clients.
Unfortunately, the rules tend to change over time, and there are several versions and interpretations of the coding guidelines. It is possible that different payers, different types of payers, and different states may enforce their own interpretations of the rules for coding. In a given state, for example, Workers Comp carriers may interpret the rules differently from Group Health payers. For this reason, the EMR does not directly code visits, but provides coding feedback during the charting process, so that providers (or professional coders on staff) can determine the correct E/M code for each individual visit. It is the client's responsibility to ensure that the final coding is correct, regardless of the feedback that the EMR is able to provide.
Broadly speaking, E/M Services are divided into general categories, depending upon the nature of the medical organization and the nature of the patient encounter. In the outpatient/ambulatory care domain that applies to the broad categories that include office visits, consultations, preventive medicine services and case management services.
CMS further divides these categories of service into subcategories, and within each subcategory there are defined levels of service coding, each represented by a CPT code. For office visits, the subcategories and CPT codes include new patient visits (99202-99205) and established patient visits (99211-99215). Preventive medicine services are likewise divided into new patient (99381-99387) and established patient (99391-99397) subcategories. The subcategories of consultations and case management services that apply to outpatient clinics are office consultations (99241-99245) and telephone calls (99371-99373), respectively.
The rules for arriving at a specific CPT code vary, depending upon the category and subcategory. The following sections describe the general coding process related to each of the four general areas applicable to office visits, office consultations, preventive medicine services and telephone calls. The application uses visit categories to know which type a visit is. When you set up the related visit categories, you will need to set the "Result Type" for each category properly, as explained in each related section below.
Office Visits
Office visits are probably the most common types of visits handled by Net Health Employee Health and Occupational Medicine users, as well as the most complex to evaluate. The application goes to great lengths to determine all aspects of coding evaluation for these visits.
Step 1: New versus Established
The first step in evaluating an office visit is to determine whether the patient is a "new" or "established" patient. A "new patient", as defined by Medicare, is someone whom you have not seen within the past three years. This is how new versus established is determined for Group Health and Family Practice (i.e. Private Practice). Workers Comp carriers have created a variation in this definition: an initial injury visit is treated as a "new patient", whereas a follow-up visit is treated as "established". For Urgent Care centers, several states have agreed to treat "new" versus "established" in the same manner as Workers Comp, while others rely upon the Medicare definition. In the context of Urgent Care, the Workers Comp definition is referred to as "problem based coding".
In order to determine "new" versus "established", the application uses the Visit Category "Result Type". These are defined as follows:
|
Result Type |
Evaluates As |
Applies To |
|
New Patient Visit |
New |
All Private Practice |
|
Established Patient |
Established |
All Private Practice |
|
New Injury/Problem |
New |
Work Comp/Urgent Care |
|
Injury/Problem Follow-Up |
Established |
Work Comp/Urgent Care |
When recording an office visit, you should select the Visit Category code that is set to trigger the Result Type that is appropriate. Note that the new injury and follow-up result type will require an Incident record, whether you are dealing with a Work Comp "Case" or with and Urgent Care "Problem". The Net Health Employee Health and Occupational Medicine EMR will then evaluate for the appropriate subcategory.
Step 2: Level of Coding
Once the New versus Established determination has been made, the second step in evaluating a visit is to determine the extent of history obtained, the extent of examination performed and the complexity of medical decision making (MDM). Each of these areas contains its own calculation rules.
Extent of history (1995 and 1997 Guidelines only)
Broadly speaking, the extent of history is determined by: (1) the count of elements documented for history of present illness (HPI); (2) the count of patient medical histories (PMH) obtained (personal past history, family history, and/or social history); and (3) the number of systems reviewed in a review of systems (ROS). Taken together, and depending upon whether this is a new or established patient, these three counts determine the level or extent of history obtained. During the charting process, Net Health Employee Health and Occupational Medicine keeps a count of HPI elements, PMH elements and ROS systems, to give the exact extent of history.
Extent of examination (1995 and 1997 Guidelines only)
The extent of examination is determined by: (1) the number of organ systems and body areas examined; and (2) the number of specific elements, often called "bullet points", either within one organ system or across organ systems. These rules vary between the 1995 and 1997 guidelines. In most cases the 1995 guidelines are more lenient. In some cases the 1997 guidelines produce better coding results. The Net Health Employee Health and Occupational Medicine EMR attempts to apply both sets of guidelines to determine the extent of examination performed. During the charting process, Net Health Employee Health and Occupational Medicine uses the number of bullet points assigned to the exam wizards and templates, as well as the count of organ systems and body areas reviewed, to give the extent of examination performed. If the wizards and template items are properly flagged with the correct number of bullet points, this will be an exact determination.
Complexity of MDM
The complexity of MDM is measured by: (1) the number of problems addressed and/or management options that must be considered; (2) the amount and complexity of medical records, diagnostic tests and/or other information that must be obtained, reviewed and analyzed; and (3) the risk of significant complications, morbidity and/or mortality, associated with the presenting problems, diagnostic procedures, and/or management options. (A table of risk is provided at the end of this topic.)
Because of the judgment required, as well as the complexity of the rules in the MDM area, Net Health Employee Health and Occupational Medicine gives the best approximation of this section. During the setup process, the provider can assign risk levels, problem and diagnostic test counts, and other factors such as chronicity, to the EMR wizards and template items. During the Net Health Employee Health and Occupational Medicine EMR charting process, the provider can override certain of these factors, based upon his/her expert knowledge, to make the level of MDM complexity more exact, if something is not accounted for properly by the automatic calculations.
The final rule for determining the coding level is listed in the table below (1995 and 1997 Guidelines only):
|
New Patient CPT Code: |
All 3 Levels Required: |
|
99201 |
Problem focused history Problem focused exam Straightforward medical decision making |
|
99202 |
Expanded problem focused history Expanded problem focused exam Straightforward medical decision making |
|
99203 |
Detailed history Detailed exam Low complexity medical decision making |
|
99204 |
Comprehensive history Comprehensive exam Mod complexity medical decision making |
|
99205 |
Comprehensive history Comprehensive exam High complexity medical decision making |
|
Est Patient CPT Code: |
Any 2 of the 3 Levels Required: |
|
99211 |
Any visit of minimal level, nurse or MD |
|
99212 |
Problem focused history Problem focused exam Straightforward medical decision making |
|
99213 |
Expanded problem focused history Expanded problem focused exam Low complexity medical decision making |
|
99214 |
Detailed history Detailed exam Mod complexity medical decision making |
|
99215 |
Comprehensive history Comprehensive exam High complexity medical decision making |
2021 Guidelines for New and Existing patients
To view the 2021 Guidelines, click HERE.
Office Consults (Remains the same for 1995, 1997, and 2021 Guidelines)
Office consults follow exactly the same rules as New Patient office visits, for purposes of E/M coding, regardless of whether the patient is technically a new or established patient. The Net Health Employee Health and Occupational Medicine EMR goes to great lengths to determine all aspects of coding evaluation for these visits.
Step 1: Office Consult Visit Category
To trigger E/M evaluation for an office consult, you must use a Visit Category code specifically for Office Consult visits that has its Result Type set to "Office Consult".
Step 2: Level of Coding
|
Office Consult CPT Code: |
All 3 Levels Required: |
|
99241 |
Problem focused history Problem focused exam Straightforward medical decision making |
|
99242 |
Expanded problem focused history Expanded problem focused exam Straightforward medical decision making |
|
99243 |
Detailed history Detailed exam Low complexity medical decision making |
|
99244 |
Comprehensive history Comprehensive exam Mod complexity medical decision making |
|
99245 |
Comprehensive history Comprehensive exam High complexity medical decision making |
Preventive Medicine Services (Remains the same for 1995, 1997, and 2021 Guidelines)
The evaluation of Preventive Medicine Services is based strictly upon the age of the patient, and whether the patient is new or established, using the Medicare definition. The Net Health Employee Health and Occupational Medicine EMR does not attempt to calculate the exact CPT code, but will display the choices to the provider. Likewise, the Net Health Employee Health and Occupational Medicine EMR does not attempt to give any feedback during the charting process, but assumes that the provider is following some currently accepted clinical guideline for the type, age and sex of the patient.
Step 1: Preventive Medicine Visit Category
To trigger E/M evaluation for an office consult, you must use a Visit Category code specifically for Preventive Medicine that has its Result Type set to "Preventive Medicine". Net Health Employee Health and Occupational Medicine does NOT attempt to decide whether the patient is new or established.
Step 2: Level of Coding
|
New Patient CPT Code: |
Coding Decision Criteria |
|
99381 |
Initial comprehensive preventive medicine: infant |
|
99382 |
Early childhood: 1 through 4 years |
|
99383 |
Late childhood: 5 through 11 years |
|
99384 |
Adolescent: 12 through 17 years |
|
99385 |
18 - 39 years |
|
99386 |
40 - 64 years |
|
99387 |
65 years of age and older |
|
Est Patient CPT Code: |
Coding Decision Criteria |
|
99391 |
Periodic comprehensive preventive medicine: infant |
|
99392 |
Early childhood: 1 through 4 years |
|
99393 |
Late childhood: 5 through 11 years |
|
99394 |
Adolescent: 12 through 17 years |
|
99395 |
18 - 39 years |
|
99396 |
40 - 64 years |
|
99397 |
65 years of age and older |
Telephone Calls / Telemedicine (Remains the same for 1995, 1997, and 2021 Guidelines)
Telephone calls by a physician to a patient, or for consultation or medical management purposes with other health care professionals, can be logged into Net Health Employee Health and Occupational Medicine as a special Telephone Call encounter. To do this, you must have a Visit Category Code specifically for Telephone Calls with its Result Type set to "Telephone Call". (These encounters are not logged in the standard visit logging area, but are logged from the Charting section of the Home Nav Bar directly by the provider. Read the topic on Telephone Calls to learn more.)
Telephone calls are evaluated by the provider based primarily upon the amount of time the call takes. There are three CPT levels. The Net Health Employee Health and Occupational Medicine EMR will provide the list, and the provider can choose the proper CPT code to use, based upon his or her judgment of the length or complexity of the call. Providers should use the local time guidelines with which their payers agree.
|
Telephone CPT Code: |
Coding Decision Criteria |
|
99371 |
Simple or brief |
|
99372 |
Intermediate |
|
99373 |
Complex or lengthy |
Table of Risk
Following is the table of risk used by the 1995 and 1997 guidelines, for evaluating risk levels for office visits and consults. These can be used as a reference for setting risk factors in Charting Wizards and template items.
Table of Risk
|
Level of Risk |
Presenting Problem(s) |
Diagnostic Procedure(s) |
Ordered Management Options Selected |
|
Minimal |
|
|
|
|
Low |
|
|
|
|
Moderate |
|
|
|
|
High |
|
|
|
(Taken from AMA CPT Professional Edition, AMA)
E/M Calculations Set Up
For the E/M calculations to work correctly, certain set up information must be entered, usually on Wizards, but sometimes on a Template. Your Net Health Employee Health and Occupational Medicine EMR came with a number of templates and wizards already created with E/M related information. However, since the interpretations of coding guidelines might vary among payers from place to place to some degree, you should review these start-up templates and wizards to make sure they are consistent with your practices.
The following fields related to E/M factors can be entered on the indicated Wizard and Template screens. If a Template Element calls a Wizard, the indicated factor is taken from the Wizard setup and cannot be changed on the Template setup.
-
Chronicity: (Entered on Template Elements and Wizards in these locations: HPI/Presenting Problems, PMH/Major & Chronic Illnesses, Assessment/Problem Assessment.) It speaks to the risk level associated with this particular step since the provider must consider chronic conditions not related to the current complaint when making decisions. In setting up Templates and Wizards, the default Chronicity can be set on a drop-down box with a list of options allowing the step to be designated as chronic, acute, self limiting. When a Wizard is being executed, the default Chronicity can be overridden with a set of radio buttons. The cumulative total of chronic problems is displayed in Number of Chronic Conditions on the ASSESSMENT tab. It can also be overridden at that point.
-
This counts as ? Presenting Problems: (Entered in Problem Assessment Wizards and the ASSESSMENT tab of Templates.) The level of complexity of the visit depends on the total number of Presenting Problems from all steps which have a number entered in this field.
-
Counts as ? Diagnoses/Options for evaluating the complexity of the MDM: (Entered inProblem AssessmentWizards and the ASSESSMENT tab of Templates.) The level of complexity of the visit depends on the total number from all steps with a number entered in this field.
-
This counts as ? sources of Data for purposes of evaluating MDM Complexity: (Entered in Diagnostic Tests and Other Data Sources Wizards on the ORDERS tab of Templates.) Data sources can include lab tests, radiology and requests for the patient chart from other providers. More data sources mean greater complexity for the visit.
-
Count this as ? bullet points: (Entered in Organ Systems and Musculoskeletal Wizards and EXAM tab of Templates.) The more bullet points that are documented, the greater the extent of examination performed.
-
MDM Risk Level: (Entered in Assessment, Medication and Procedures Wizards and the related tabs on templates.) The choices are N/A, Minimal, Low, Moderate, and High. Medical Decision Making (MDM) area
Coding multiple elements
In certain EMR charting situations, providers and clinicians need to document items or findings that overlap multiple categories or elements. For example, part of a note might encompass two organ systems in the Review of Systems, or an interim history note might cover multiple elements in the History of Present Illness area. Net Health Employee Health and Occupational Medicine has the ability for users to set up wizards that overlap multiple elements, and thereby allow Net Health Employee Health and Occupational Medicine to count all of those elements at the time of charting. Thus, for example, a single wizard in the HPI area can be set up to give E/M credit for location, duration, timing, severity and quality, all at the same time, if appropriate.
In conjunction with the ability to set up wizards for multiple element credit, the free text wizard also allows users to check off all of the affected elements at the time of execution. For example, while entering free text for personal history, the user can elect to give credit for both personal and family history.
This enhancement is most useful in the subjective information tabs (HPI, PMH and ROS).
Coding multiple elements using Wizards under 2021 E&M Coding Guidelines
The 2021 E&M Coding Guidelines have changes that allows billing to occur based on patient visit time.
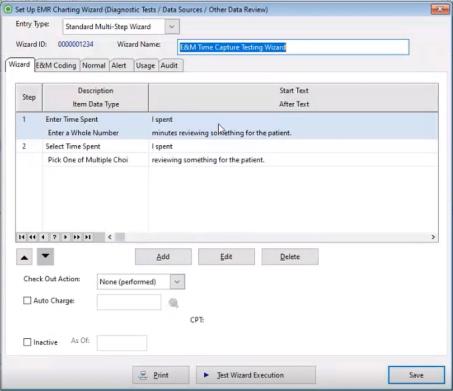
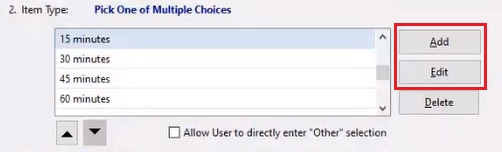
Click Add to create a new wizard.
If you are using 2021 E&M coding guidelines, there are two selections you may choose for the dropdown menu in the field Fill-In Data Type:
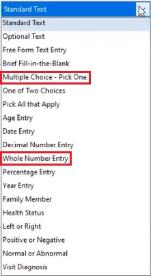
Multiple Choice - Pick One

This choice allows you to enter Face-to-Face patient visit time through specified 15 minute increments. Non-Face-to-Face patient visit time can be attached to each 15 minute increment by selecting the Add or Edit button. The "Minutes of Non-Face-to-Face time" may vary and only needs entered according to what the prompt says.
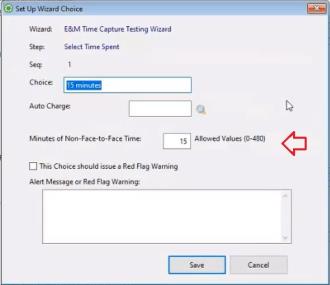
Enter the minutes associated with the interval choice in the Minutes of Non-Face-to-Face Time field.
Click Save on the Set Up Wizard Choice.
Click Save on the Set Up EMR Charting Wizard Step window.
Whole Number Entry

This choice allows you to enter whole numbers for Non-Face-to-Face patient visit time. Non-Face-to-Face patient visit time can be included by selecting the Count as Non-Face-to-Face time for E&M checkbox.
Click Save on the Set Up EMR Charting Wizard Step window.
User Choices
During the Net Health Employee Health and Occupational Medicine EMR charting process, the provider can override E/M factors, based upon his/her expert knowledge, to make the level of MDM complexity more exact, if something is not accounted for properly by the automatic calculations. For example, Net Health Employee Health and Occupational Medicine might not recognize that there are two or more problems involved, involving a higher risk level. (The recognition of risk sometimes depends upon multiple factors at play.) Also, the value of the count of problems can depend upon intangible factors, such as whether it is new or existing, fully diagnosed or requires additional workup. Being somewhat intangible, they might not be recognized by the software calculations.
The area of the software that you may need to override the Net Health Employee Health and Occupational Medicine calculations is in the evaluation of complexity of MDM. The tabs where changes can be made are ASSESSMENT and ORDERS.