How to Set Up a Provider Network
Workers Comp Medical Provider Networks
The State of California now requires all employees to choose a medical provider network (MPN). To accommodate this requirement, the software now allows you to associate an MPN with the employee on the [Enter Patient (patient name/company name] window. (This field is not available on the Enter Patient (patient name / Private Practice) window. The network will be captured with Workers' Comp visits, and visit, referral and revenue reporting can be reported by network. In addition, you can map providers to provider networks to assist in your work flow.
Private Practice Provider Networks
The program also has the ability to establish networks of providers for use in certain Private Practice situations, along with special provider network fee schedules. A provider network is created for a specific carrier. Multiple providers can be associated with each network (available for information purposes only).
Provider networks are set up first from the Setup/Admin, under the provider entity section of the ENTITY CODES sub-tab. During that process, providers and a carrier can be linked. Also, during the process, a fee schedule can be set up for that network. Like the billing account override fee schedule, a standard discount percentage can be assigned, and/or individual charge overrides can be set up. When charges are processed during invoicing, if there is a special price for a provider network, that price is used for that patient.
To activate a network for a particular visit, the network should be associated with the patient as part of setting up a group health insurance record. Whenever a private practice injury visit is logged for the patient, the network will be captured in the visit and used to determine fees. The network will flow all the way through billing and into sales analysis.
Provider network fee schedules
Any provider network can have its own special fee schedule. When a visit is recorded with which a provider network has been associated (whether for Workers Comp or Private Practice / group health), any service items for which a special fee has been set up will be priced using that override fee. Setting up a network fee schedule follows a similar pattern to what is employed for pricing with individual billing accounts and contracts. You can elect to use standard pricing, a standard discount (or premium) percent, or override prices on an individual item basis. Since insurance companies often have a number of provider networks, it might be easiest to enter the fee schedule for one and then transfer it to others, thus reducing the amount of work required.
Set Up Provider Networks
Add a Provider Network
Provider networks are added from the Select Provider Network window. There are two points from which this screen can be reached:
-
On the Home Nav Bar , then , then button. Or,
-
Select Setup / Admin
-
Select Providers
-
Select Provider Networks
OR
-
On the Home Nav Bar
-
select Setup / Admin
-
select 3rd Party Payers
-
Select Carriers
-
Search for and select the carrier you want
-
The Enter Insurance Carrier window opens
-
Select the Organizations tab
-
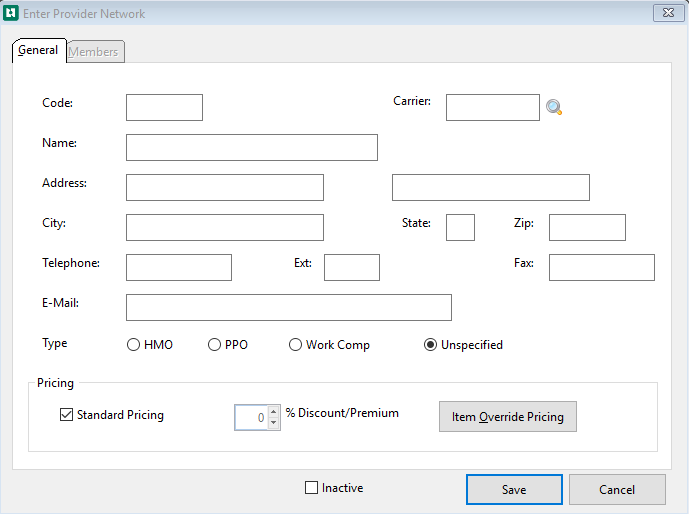
Select Add to display the Enter Provider Network window.
-
Enter a Code for the network.
-
If you are entering this provider network from the Enter Insurance Carrier window, the carrier will already be displayed in the Carrier field. If not, and if the provider network is associated with a carrier:
-
Select the magnifying glass
 beside the Carrier field.
beside the Carrier field. -
The Select Insurance Carrier window opens
-
Search for and select the correct carrier.
-
-
Enter name, address, and contact information.
-
Select a Type.
-
HMO
-
PPO
-
Work Comp
-
Unspecified
-
-
Pricing
-
Select Standard Pricing to use the fees assigned to the carrier
-
Use % Discount Premium to add a percentage to be assigned to the charges
-
Use Item Override Pricing to enter different prices for items
These fields work the same as the fields of the same name on the PRICING AND INVOICING tab of the Billing Account.
-
-
Select the Members tab.
-
To add members to the network select Add.
-
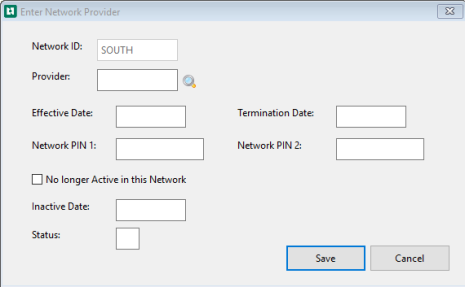
On the Enter Network Provider window select the magnifying glass beside the Provider field.
-
Search for and select the provider.
-
Fill in the additional fields, as required. These fields are for reference only-the software does not use them in any way.
-
Select Save
Add a Provider to a Provider Network
-
On the Home Nav Bar, click Setup / Admin.
-
Select Providers.
-
On the Setup Providers/ Practitioners bar, select Providers
-
The Select Provider window opens
-
Search for and select the provider you want.
-
Select the Billing tab.
-
Below the Provider Networks to which this Provider Belongs pane
-
Select Add
-
The Enter Network Provider window opens
-
Select the magnifying glass beside the Network ID field.
-
The Select Provider Network window opens
-
Search for and select the correct network.
-
Fill in additional fields as required. These fields are for reference only-the program does not use them in any way.
-
Select Save
Enter a Provider Network for a Patient
-
On the Home Nav Bar
-
Select Demographics
-
The Patient Search pop-up window opens
-
Enter the Last Name and First Name, and Birth Date
-
Select OK
-
The Select Patient window opens
-
The search will provide a list of whatever matches the information entered on the Patient Search window
-
-
Search for and select the patient you want.
Make sure to check Select Private Practice check box, not as an Occupational Medicine employee.
-
Click the Insurance tab.
-
If the patient's health insurance carrier has not been added, click Add. Read How to Add Patient Insurance to learn about completing this screen.
-
If the patient's health insurance carrier has been added, select Edit.
-
-
Select the magnifying glass
 beside the Network ID
beside the Network ID -
Search for and select the correct network.
-
Fill in additional fields as required.
-
Select Save
The Medical Provider Network can also be entered on the Insurance tab of the Enter Visit window. Select the Payer by double clicking or selecting Edit. Then follow steps 9 through 12.
Provider Network Fee Schedules
Steps to set up a provider network fee schedule
-
On the Home Nav Bar
-
Select Setup / Admin
-
Select Providers
-
The Setup Providers / Practitioners sub menu opens
-
Select Provider Network
-
Select the Provider Network to set up the Provider Network fee schedule
-
Locate the Provider Network to have the fee schedule created
-
Select Edit
-
The Enter Provider Network window opens
-
Under Pricing select Item Override Pricing
-
The Provider Network Fee Schedule (provider Network name) window opens
-
Locate all of the items that need an override fee.
-
Double click or select Change to open the item
-
Enter Network Fee window opens
-
A charge for Current or Future can be entered along with an Effective Date.
If the fee will go into effect at a future date, enter it in the Future override fee field. Then enter the date when the fee goes into effect. the program will automatically start using the fee on that date. Future dates will not be displayed on the [Provider Network Fee Schedule] window, only current ones. When effective date fees are entered, a process must be carried out after the effective date to move the future fee into the current fee field, clearing out the future fee for the next round of updates. Read the topic on Effective Date Pricing to learn more.
-
A no charge check box is also available
-
Select Save
-
On the [Select Provider Network] window search for and select the provider network for which you want to enter a fee schedule. (The network must be created before the fee schedule can be entered.)
-
Click OK.
Print the fee schedule
To print the fee schedule, click the Print button in the lower right side of the Provider Network Fee Schedule locator window.